An estimated 1 in 3 women and 50% of mothers who have given birth will experience some form of prolapse. Yet so many women we see at The Wellness Boutique don’t know about the condition or are surprised when things ‘down there’ change through ageing or postpartum.
June is Pelvic Organ Prolapse (POP) Awareness month, so we’re here to shed some light on this women’s health issue and educate you on ways to manage it effectively if you are experiencing symptoms.
What is Pelvic Organ Prolapse?
Pelvic Organ Prolapse is a condition where internal pelvic organs, including the bladder, uterus and bowels, descend into, or out of, the vagina.
In simple terms a prolapse means there has been an increase in laxity (looseness) in the fascia and ligaments. The muscles can’t do their job properly without the strength of these support structures.
POP can impact bladder and bowel control and cause discomfort and embarrassment. But as we mentioned, it’s surprisingly common and with support, can be managed so women don’t experience unnecessary discomfort and bothersome symptoms.
Risk factors
There are a few factors that increase women’s chances of experiencing prolapse, including:
- Pregnancy and childbirth (particularly forceps assisted vaginal delivery).
- Chronic constipation (all that straining can put pressure on your supportive pelvic floor tissues).
- Chronic coughing (this places ongoing pressure on the pelvic floor).
- Health conditions like cystic fibrosis and emphysema (due to persistent coughing).
- Genetic predisposition (evidence suggests a slightly increased risk if it runs in the family).
Types of prolapse
There are three main types of prolapse. Women can experience one or a combination of all three, including:
- Anterior wall (formally called cystocele), where the bladder pushes on the wall of the vagina.
- Posterior wall prolapse (formally called rectocele) where the bowel pushes onto the wall of the vagina.
- Uterine prolapse where the uterus slips down and pushes into the vagina.
Stages of prolapse
There are four different stages of prolapse:
Stage 1 and 2 – Mild to moderate
The organs aren’t protruding outside of the vagina in these stages, and the prolapse can usually be managed conservatively.
Stage 3 and 4 – Slightly more severe
The organs are descending outside of the vagina. These stages will often require the support of a pessary or, in some cases, surgery to manage the prolapse.
Signs and symptoms
If you are experiencing any of the following signs of prolapse, it’s worth seeing a qualified women’s health physio for an assessment. The earlier you know about a potential prolapse, the easier it will be to manage it in the long term. Signs and symptoms of prolapse include:
- A heavy sensation including a feeling of dragging in the vagina.
- A bulging that you can see or feel within or outside of the vagina.
- Bladder or bowel not fully emptying (you may notice dribbles or be surprised that you need to return to the toilet even when you think you’re finished).
- Pain, decreased sensation, or difficulties during intercourse.
- Recurring urinary tract infections.
Things you can do to manage prolapse
Taking proactive steps as soon as you notice symptoms will reduce pain and discomfort and help restore the integrity of your pelvic organs. While prolapse doesn’t heal naturally, the good news is they can be successfully managed with a personalised treatment plan and the proper support.
Steps you can take to begin your healing journey:
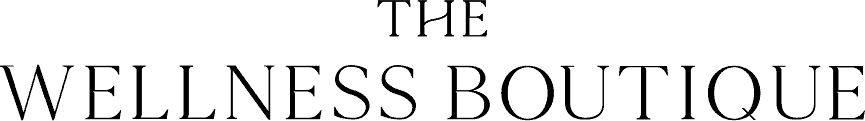
- Schedule an assessment with a qualified women’s health physio.
- Learn about your condition (prolapse type, stage, triggers and habits).
- Get an individualised treatment plan suited to your needs.
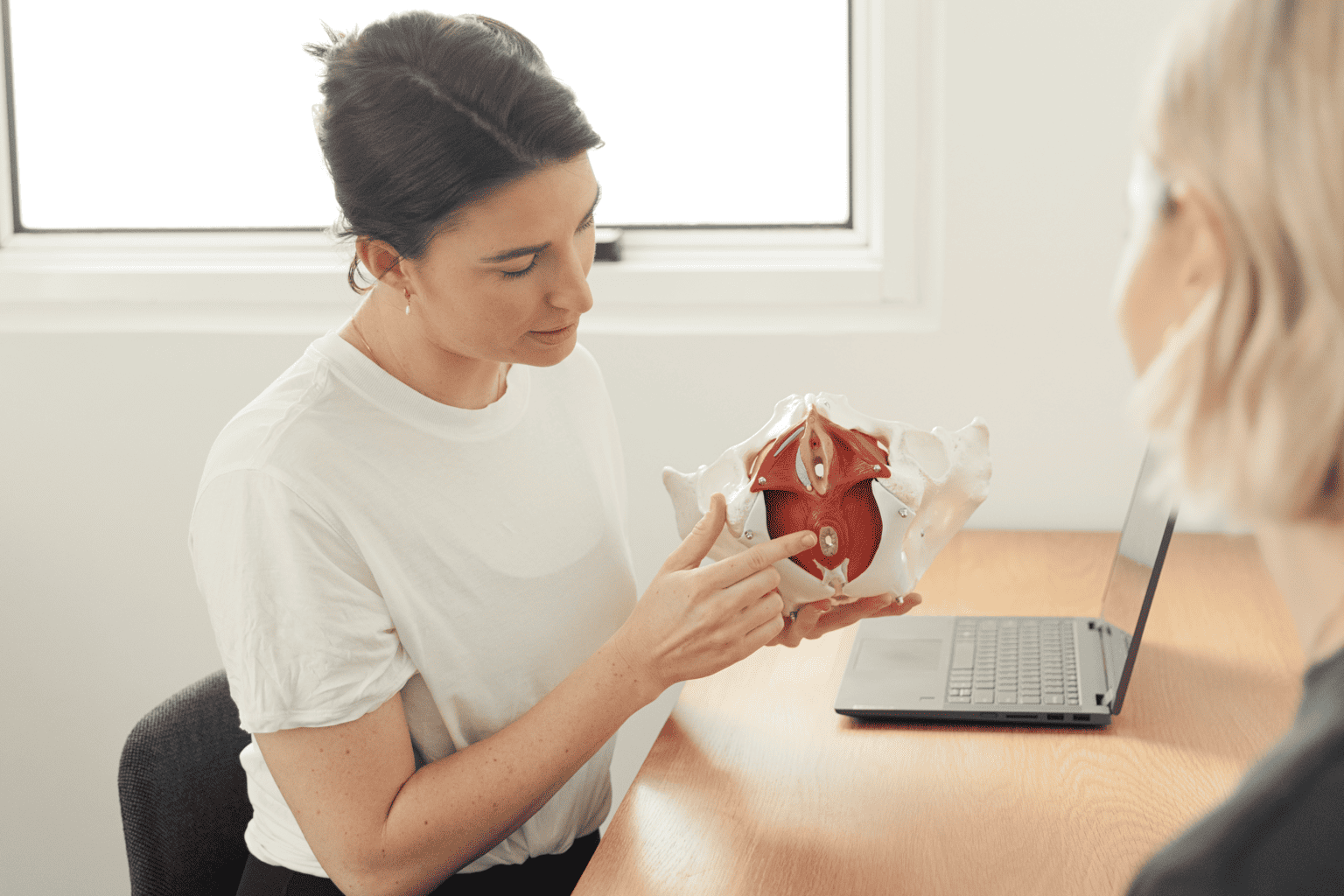
- Strengthen your pelvic floor muscles with tailored exercises.
- Try optimal bowel techniques to alleviate straining on the toilet.
- Nourish your immune system to avoid colds and coughs that cause added pressure.
- Implement strategies to safely manage strain on your body e.g., adjust techniques during physical activity like running or weights.
- Keep active to maintain a healthy weight (even 3-5kgs weight loss can have a positive impact).
- Get a custom pessary (a medical-grade silicone device) professionally placed into your vagina to provide internal structural support.
- Consider surgery if advised by your gynaecologist or physio and if your condition is severe.
As you can see, there is so much value and knowledge a supportive women’s health physio can offer you if you suspect you are experiencing some symptoms of prolapse.
We love to empower women with the understanding and confidence to ask questions, get answers and manage their health conditions to live a great life.
If you are pregnant, we recommend booking into our birth preparation program with one of our qualified women’s health physios to prepare your pelvic floor for birth. And if you are a woman of any age experiencing symptoms of prolapse, book a pelvic floor assessment with one of our experienced senior physiotherapists to create your custom care plan.